Daily photo update
January 2025 fly-over video update
Moses Lake Community Growth.
Samaritan Healthcare was formed in 1947, giving Samaritan Hospital, Public Hospital District #1, a 75-year history of being a community hospital—owned and governed by local citizens.
As the area continued to grow, the hospital board of commissioners agreed to construct a new hospital on Samaritan’s current site and it opened in 1955. Over the years, Samaritan Healthcare has deliberately chosen to keep our healthcare local as we provide care and services that are tailored to meet the unique needs of our communities.
Today, Moses Lake and the surrounding area continue to grow, both in population, as well as in various industries and the services offered to our residents. Since 2010, Moses Lake’s population has grown 80% faster than Grant County and 85% faster than Washington State overall. As Moses Lake is growing into a regional community, our hospital has grown into a regional healthcare facility.

Grant County Resident Needs.
In responses to two surveys in 2016 and 2018, Grant County residents identified the top four needs to improve the community healthcare experience: more primary care and specialty providers, recruit and retain the best possible staff, modern and up-to-date facilities, and reduce the need to travel outside the area for healthcare.

Community Growth.
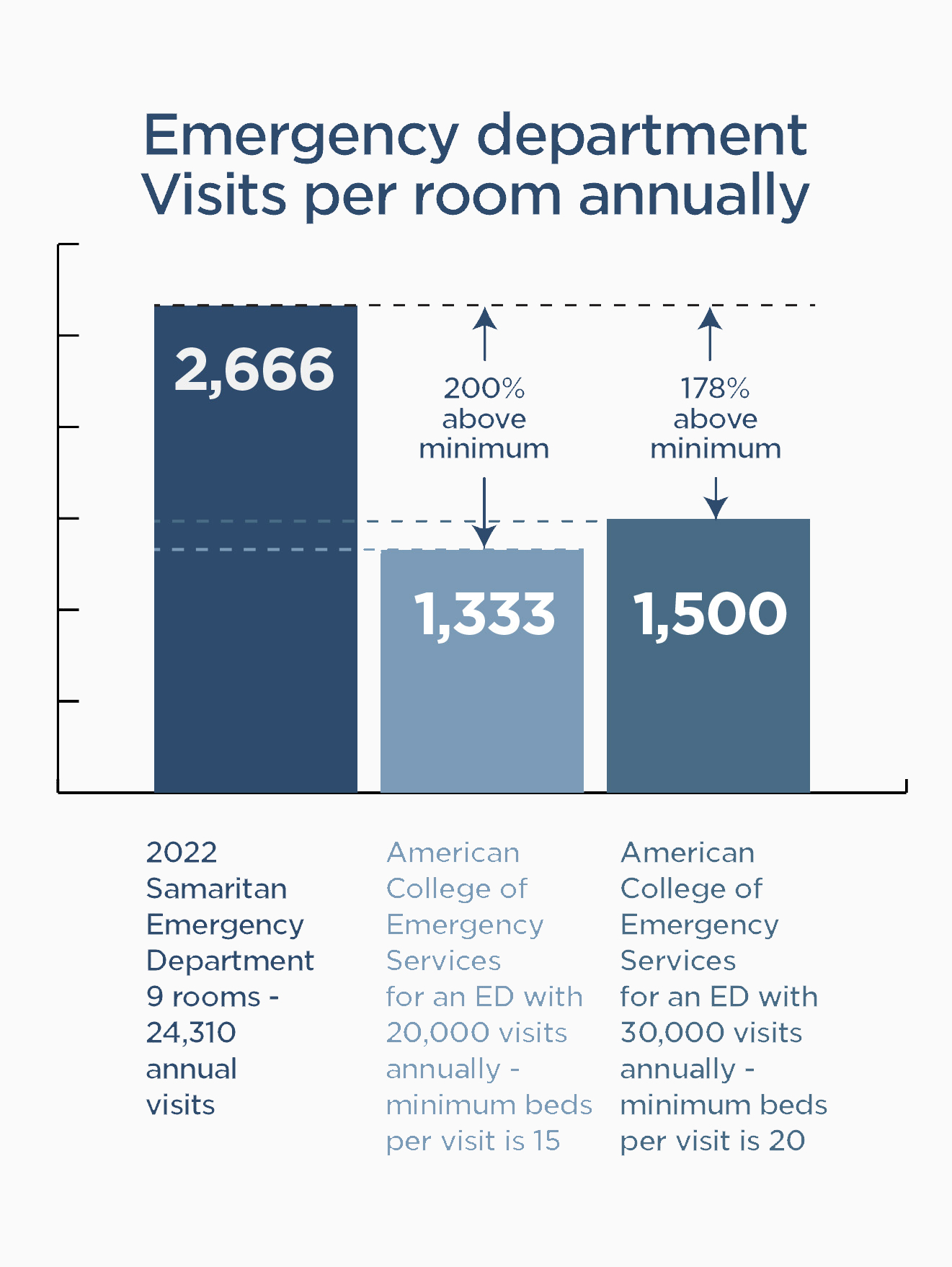
Our community is surging from a population growth perspective, and we need to plan for both today and the future. American College of Emergency Services recommends that an ED with 20,000 visits annually should have a minimum of 15 beds. Samaritan is operating significantly above these numbers—200% above the 1,333 visits per room minimum for 20,000, and 178% above the minimum for 30,000 visits.


Provider Growth.
On-staff providers have grown by 300% over the last seven years, with seven new medical specialties: Allergy, Behavioral Health, Cardiology, Diabetes Care, Gastroenterology, Neurology, and Pain Management.
Keep Our Healthcare Local.
We need to keep our healthcare local, to continue being able to better serve our patients in a timely manner, our staff needs space designed for the care they deliver. We must look ahead and provide a facility that is designed to meet the current and future needs of our community.
Realizing that a 1950s’ hospital can no longer solve the 21st-century needs of our community—Samaritan staff had been actively exploring all options. Samaritan also still holds the non-renewable USDA 2.25% low-interest loan that must be used by September 2026.
Community hospital ballot proposition.
With input from residents who attended the community open house as well as with feedback from several other local presentations, Samaritan Healthcare’s Board of Commissioners has voted unanimously to adopt a resolution requesting a ballot proposition to be placed on the ballot. The proposition asks for the community’s financial support in order to move forward with the construction of a future community hospital.
Benefits of a future community hospital:
- Keeps care local.
- Expands reliable local emergency care.
- Expands access to specialty and surgical care that stays local.
- New, first-in-class modern maternity care.
- Flexible, adaptable, and expansion-ready hospital and ICU rooms.
- A 1950s’ hospital can no longer solve the 21st-century needs of our community.

- Current ED is operating 200% above capacity


- Expansion limitations within existing hospital
The new hospital will expand the emergency department to serve our rapidly growing community and will provide specialty care to patients from Moses Lake, Warden, and Ruff, as well as an expanded emergency department (ED).
Since 2010, Moses Lake’s population has grown 80% faster than Grant County and 85% faster than Washington State overall. Samaritan Hospital’s Emergency Department (ED) has 9 beds and had 24,310 annual visits in 2022. The American College of Emergency Physicians recommends that an ED with 20,000 visits annually should have a minimum of 15 beds. Presently, Samaritan’s ED is operating at 200% above the recommended capacity.
“Getting patients seen as quickly as possible, especially the sickest patients as quickly as possible and either getting them back home where they can recover or upstairs in the hospital where they can begin their treatment is important to us,” said Dr. Matthew Lockwood, Medical Director of Samaritan Healthcare’s Emergency Department. “The faster we can do that, the better we can take care of patients, and the more patients we can see on a daily basis.”
“A future community hospital shows that Samaritan is committed to the health of our residents,” said Rebecca Suarez, RN, Director of Emergency Services at Samaritan Healthcare. “The ED is overcrowded more often than not and the lack of space is the biggest barrier. On days where there are a lot of patients and the ED is overcrowded it is more complicated, but we rise to the challenge. Staff are more efficient when given adequate work space, patients are placed in appropriate care areas, such as flex care, trauma room, or a main ED bed, plus the patient experience is greatly improved.”
- Surgery is operating at max capacity
- Larger surgical rooms needed for advanced surgical technology (robotic-assisted equipment)
- Seven new specialty care services since 2016
The OR/Surgery department—a medical specialty that was requested by the community in our 2016 and 2018 surveys—will be expanded and made more operationally efficient in the future community hospital. The new layout has 5 operating rooms (with one area for expansion when needed), 15 Pre/Post rooms, plus an additional 9 PACUs (Post-Anesthesia Care Unit). After receiving anesthesia for a surgery or procedure, a patient is moved to the PACU to recover and wake up.
With our Samaritan and other community-based surgeons on our medical staff and the various surgical specialties that they represent—ENT, general surgery, gastroenterology, OB/GYN, ophthalmology, orthopaedics, pain management, podiatry, and urology—a significant amount of equipment and supplies requires proper storage and space. As space requirements for equipment and robotic technology are growing, increased OR size is also greatly needed.
In the existing OR, only one surgery room has the space needed to use robotic-assisted technology. This creates a scheduling conflict when general and orthopedic surgeons both need the same room for their equipment. In the new hospital, all the surgery rooms will have the space for robotic-assisted technology, thus providing more capacity.
“In the current hospital, two of the four existing operating rooms are very small,” said M. Lyndon Dieter, MD, Perioperative Medical Director/Anesthesiologist of Samaritan Healthcare Hospital. “Even in the larger operating rooms, space is at a premium. There needs to be sufficient space for personnel, plus room to maneuver the patient.”
 985 babies delivered annually
985 babies delivered annually- Labor, delivery, recovery all in one patient room
- Advanced nursery allows at-risk mothers and babies to stay close to home in the early weeks of life
- Tele-Pediatric ICU and Tele-Neonatal ICU provide increased care for higher-risk patients
The need to update the Mother and Baby Unit is also being addressed within the design of the future community hospital by constructing a regional LDRP (labor, delivery, recovery, postpartum) with the capability of serving more than 1,000 annual births. Each room is LDRP, which means when a mother checks into a room, her entire birthing experience until she checks out will be within her own private birthing room. There will also be an advanced nursery with a higher level of care for higher-risk births. This allows mothers and babies who need this care to stay close to home and their families in the early weeks of life.
 Private patient rooms with space for family to stay overnight
Private patient rooms with space for family to stay overnight- Advanced technology in patient room for improved care
- Expansion capable by 10 additional hospital rooms as community grows, meeting the needs of your family through your healthcare experience
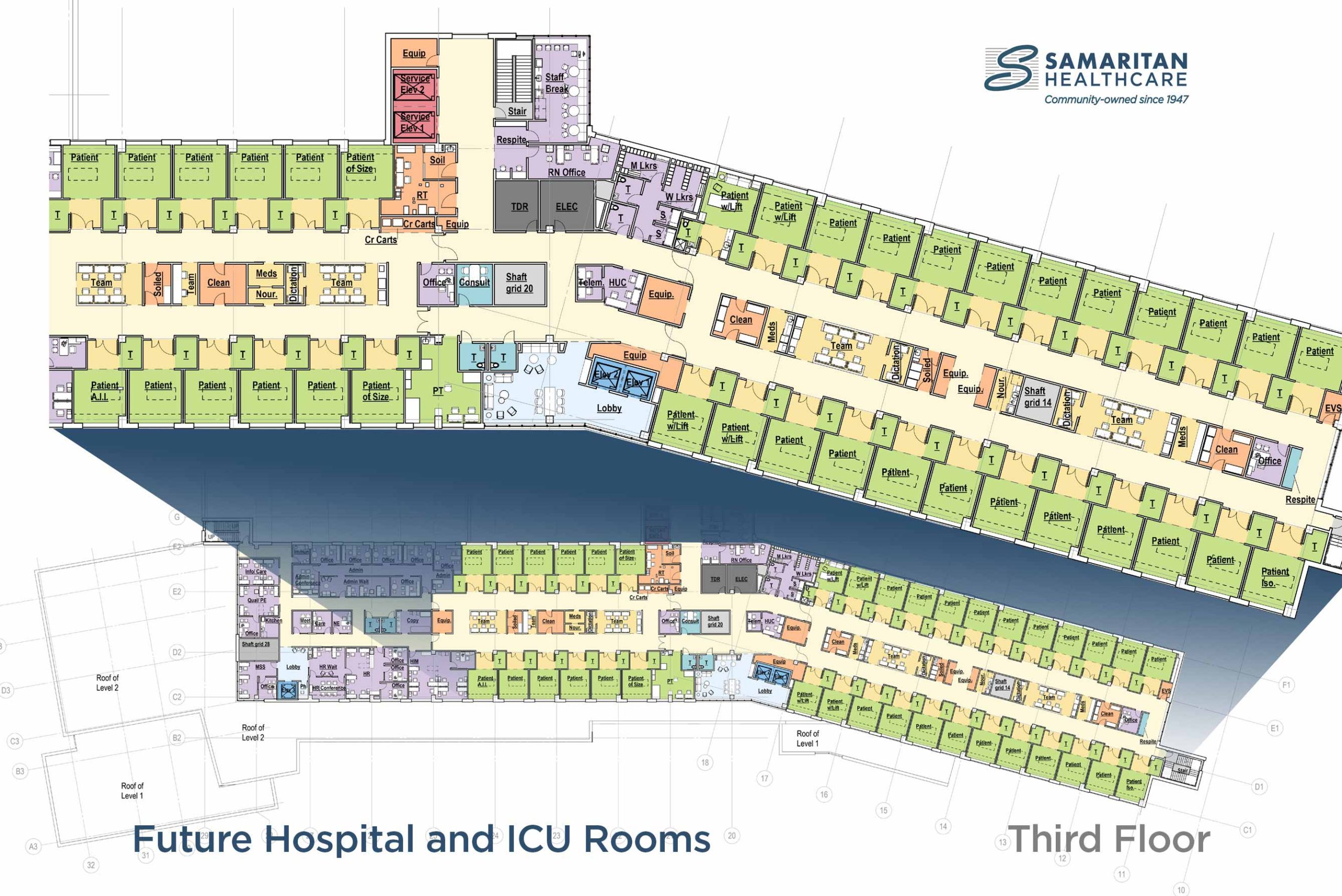
Surgery and the Emergency Department are all adding rooms. The patient/hospital rooms and ICU rooms will be flexible and adaptable to meet the needs of your family throughout your healthcare experience. Patient rooms and ICU rooms are all on the same floor and have the same technology. When needed, an ICU room can become a hospital room and a hospital room can become an ICU room.
Private patient rooms have space for family to stay overnight when conditions allow, and will have advanced technology within the room for improved care. With today’s technology, more surgical patients are going home the same day (outpatient). If needed, there will also be space for expanding with 10 additional patient rooms in the new hospital as the community grows
- Our growing community: population, businesses, hospital use
- Community care needs (surveys)
- Current hospital facility limitations
In responses to two surveys in 2016 and 2018, Grant County residents identified the top four needs to improve the community healthcare experience: more primary care and specialty providers, recruit and retain the best possible staff, modern and up-to-date facilities, and reduce the need to travel outside the area for healthcare.
Since the last major addition/renovation to Samaritan Hospital was more than 20 years ago, the delivery of healthcare has changed—including requiring more room for patients, equipment for medical/technology needs, supplies, and more.
“While the existing hospital is clean, visually appealing, and appears functional, the mechanical components of the facility—boilers, chillers, HVAC, generators, etc., are at their maximum capacity,” said Theresa Sullivan, CEO, Samaritan Healthcare. “The mechanical aspects are at the end of useful life, with no capacity for expansion. New equipment is a responsible investment in our operational efficiency. It would allow our future community hospital to operate at a reduced cost when compared to our current hospital, as well as taking into consideration the costs for energy, technology, and infrastructure.”
With modern infrastructure—from mechanical and energy-efficient windows to up-to-date construction materials and design—the community’s future hospital is designed to meet the current and future needs of our community.
Community FAQs:
“Are 50 beds enough in our new hospital?”
Here’s how approval of the ballot proposition will address this concern:
The 3rd floor is designed to be flexible and can expand to 10 beds depending on patient needs. Being flexible means the ICU and patient hospital rooms are on the same floor, and are built the same. An ICU room can become a patient room, and a patient room can become an ICU room. If the ICU is full, ICU can use available patient rooms and vice versa.
The current hospital cannot be flexible because the ICU is on the 3rd floor, and patient rooms are on the 2nd floor, plus the capabilities of the rooms are different. Additionally, modern medicine allows us to send more patients home the same day after some surgeries, so there’s less need to occupy a hospital room.
“We have to get the new hospital built to have more than 50 rooms if we need them. We have been full in the hospital and there are times we are not full, but our ED and Surgery all struggle every day to have enough room,” Theresa Sullivan, CEO, Samaritan Healthcare.
“What will you do with the existing hospital?”
The next use of the building and land needs to be a community conversation that Samaritan is willing to lead. The facility and land are community assets, so we’d like to ask the community to consider what is the best use for this building to serve the community in the future.
Whoever moves into this building next will have work to do—it’s not turn-key. In addition to the purchase price of the current hospital and land, there will be additional financial costs. Since the operational systems are near their end of life, they will need updating. There will also be limitations due to the aging infrastructure as to what can be done via remodeling or construction.
“Would the property value of the existing hospital help offset the cost?”
The most recent valuation of the current hospital building and land was done by Colliers International and was stated to be in the range from $3M to $4M. However, this valuation is now three-to-four years old and could be updated for 2023 values.
What is Colliers’ area of expertise? Colliers (NASDAQ, TSX: CIGI) is a leading, diversified professional services and investment management company with operations in 63 countries. Collier’s 18,000 appraisers are held to a strict code of ethics as determined by the Uniform Standards of Professional Appraisal Practice (USPAP), which requires that all appraisals be unbiased and based on credible information.
During the appraisal process, Colliers thoroughly evaluated all the pertinent information and materials available to produce a well-supported opinion of value. All Collier appraisals are evaluated and approved by an experienced review team to ensure their clients receive clear, concise, and timely appraisals.
“Could you wait until inflation goes down to build?”
Inflation won’t last forever, but it won’t go backwards either. Commodity prices for materials and supplies are not going down in the foreseeable future. Samaritan Healthcare also still holds the non-renewable USDA 2.25% low-interest loan that requires constructing the new hospital by September 2026.
Additionally, the population of Moses Lake is growing at 23.5%, which is 85% faster than Washington State. (The State of Washington is growing at 12.7%.)
Our Emergency Department can’t wait—it’s already operating at 200% above capacity.
Surgery can’t wait either. In the existing hospital, there is only one surgical room that’s big enough to to use the robotic-assisted technology our surgeons are trained to perform—this leads to scheduling backups. We’ve grown our providers by 300% since 2016, with the vision of the new hospital being constructed.
“How much will my property taxes go up with the hospital bond?”
Samaritan Healthcare is asking for a ballot proposition to help cover only a portion of the future community hospital total cost. Of the estimated property taxes, it is estimated at $1.10 per thousand dollars of assessed property values per year.
Bonds for Public Hospital
The Commission of Public Hospital District No. 1, Grant County, Washington (Samaritan Healthcare), adopted Resolution No. 1/23-02 concerning a proposition to finance a new public hospital and related facilities. If approved, this proposition would authorize the District to construct and equip a new public hospital and carry out other capital improvements deemed necessary or advisable by the Commission; issue no more than $130,000,000 of general obligation bonds maturing within 30 years; and levy annual excess property taxes to repay the bonds, all as provided in Resolution No. 1/23-02.
Public Hospital District No. 1 (the “District”) operates Samaritan Healthcare in Moses Lake. The District has determined that its existing hospital facility does not have sufficient capacity to meet the increasing health care needs of the District’s residents and that it is essential for the public’s health and welfare that the District construct and equip a new hospital in Moses Lake.
To pay for the costs of the new hospital, the District is proposing a ballot proposition to be voted on by the voters of the District. If approved, this proposition would authorize the District to construct and equip a new hospital and carry out other capital improvements deemed necessary or advisable by the District; issue no more than $130,000,000 of general obligation bonds maturing within 30 years; and levy annual excess property taxes to repay the bonds. The average levy rate required to repay the bonds is estimated to be $1.10 per $1,000 of assessed value. For a home with an assessed value of $170,000, the average monthly tax increase is estimated to be $15.50 per month.
The remainder of the project ($100,000,000) will be paid for by a historically low interest rate loan provided by the USDA, Samaritan Foundation fundraising, and local, state and national grants.
Exemptions from taxes may be available to certain homeowners. For more information, please call the Grant County Assessor’s Office at (509) 754-2011.
* Renderings for concept only, subject to change.
Click here to download the renderings and Future New Hospital Overview (pdf)
To learn more about how to donate to the future community hospital, click here.








 985 babies delivered annually
985 babies delivered annually


 Private patient rooms with space for family to stay overnight
Private patient rooms with space for family to stay overnight